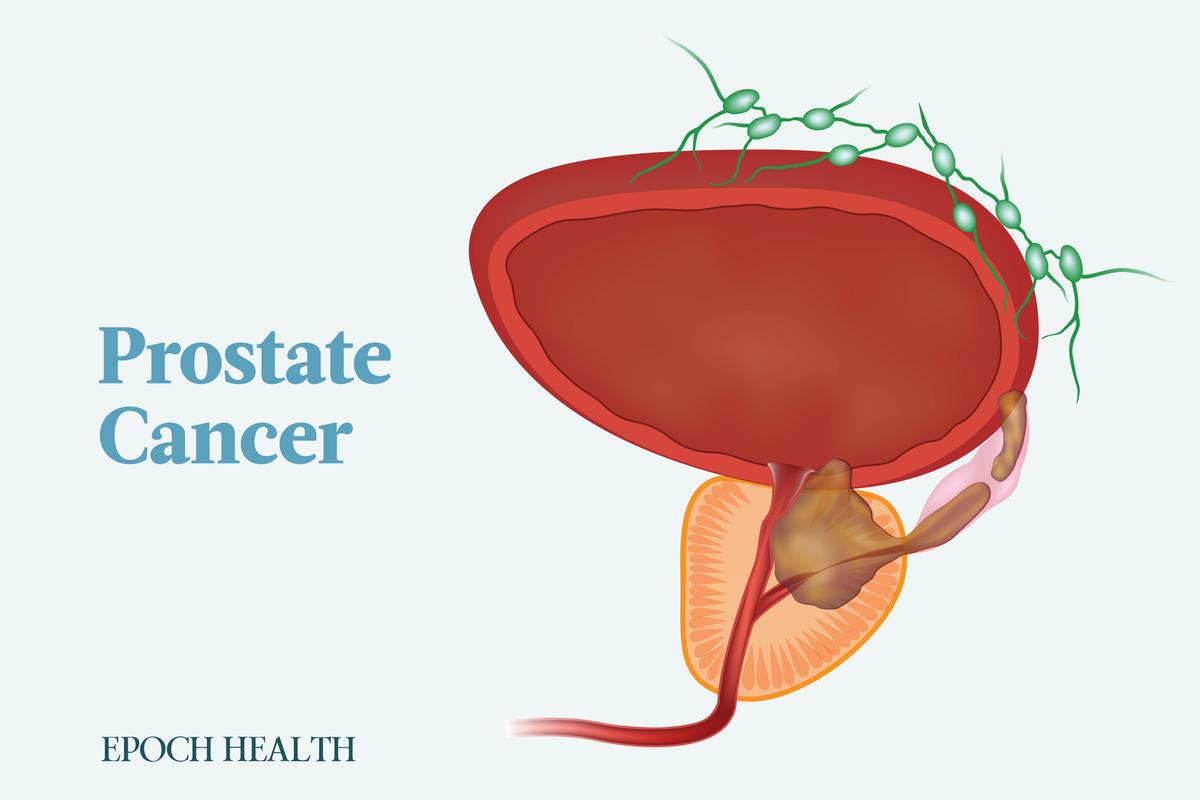
Prostate cancer occurs when abnormal cells undergo uncontrolled growth in the prostate gland, resulting in the formation of a malignant tumor. The prostate is a walnut-sized organ situated deep within the pelvis, and it plays a vital role in the production of semen, which serves to nourish and facilitate the transport of sperm.
What Are the Types of Prostate Cancer?
- Adenocarcinoma: Adenocarcinomas, the most prevalent form of prostate cancer, originate in the gland cells lining both the prostate gland and its tubes. These gland cells play a role in the production of prostate fluid. The subtype acinar adenocarcinoma makes up 90 percent of all prostate cancers and originates in the gland cells lining the prostate. The second subtype, ductal adenocarcinoma, originates in cells lining the tubes of the prostate and tends to grow more aggressively.
- Transitional cell carcinoma: Also known as urothelial carcinoma of the prostate, transitional cell carcinoma of the prostate represents 2 percent to 4 percent of prostate cancers. It originates in the cells lining the urethra, the final tube that empties the bladder during urination. Typically beginning in the bladder and spreading to the prostate, it can infrequently initiate in the prostate and extend to the bladder entrance and adjacent tissues.
- Squamous cell carcinoma: This type arises from flat cells covering the prostate and typically grows and spreads very aggressively. It makes up less than 1 percent of prostate cancers.
- Small cell: The rarest of these types, small cell prostate cancer represents less than 2 percent of all prostate cancers, and it falls under the category of neuroendocrine prostate cancer. Distinguished by rapid growth, small cell prostate cancers often present in an advanced stage at the time of diagnosis, with the cancer having spread to distant parts of the body.
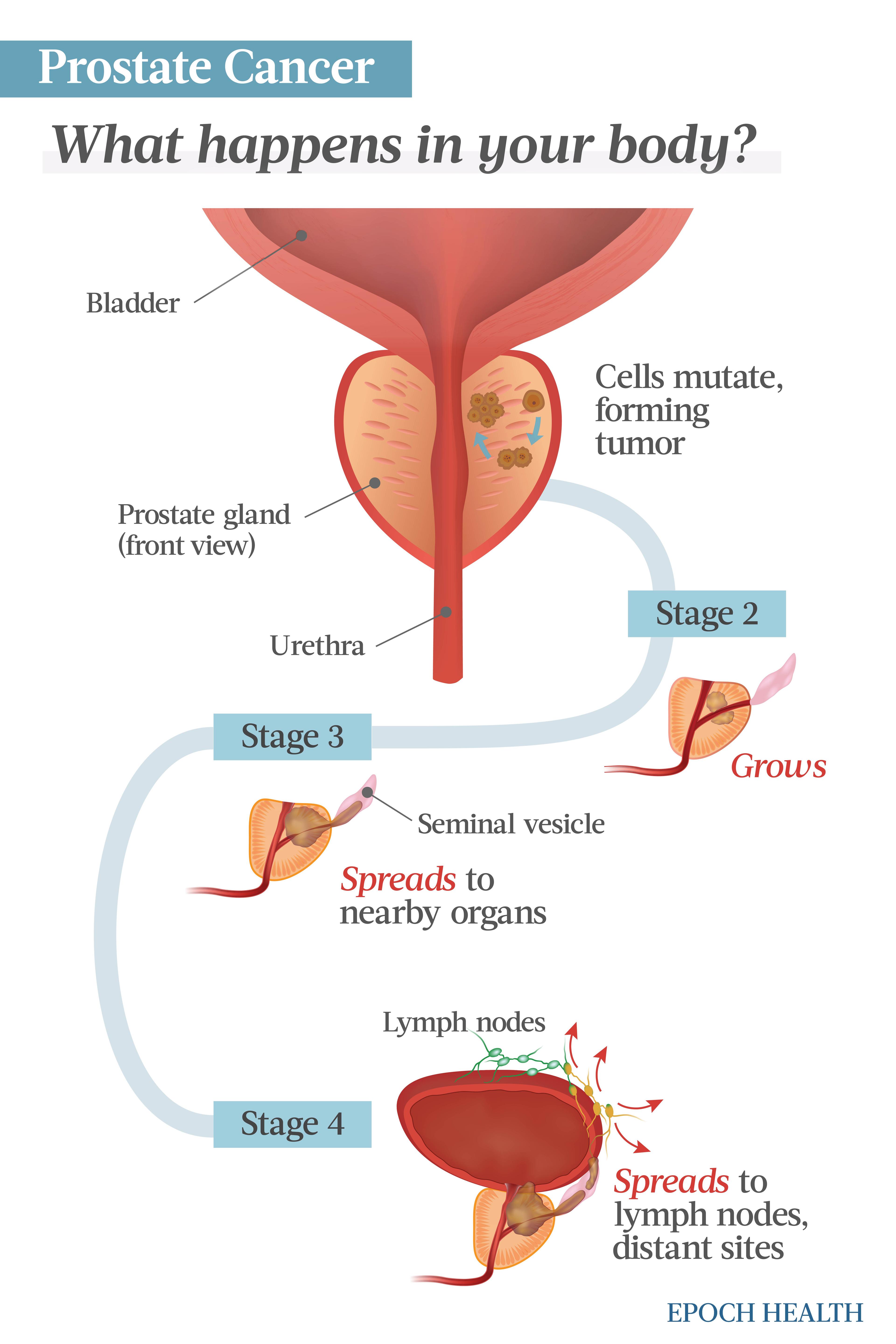
What Are the Stages of Prostate Cancer?
- Stages 1 and 2: In the early stages, the tumor remains localized within the prostate.
- Stage 3: The cancer has extended beyond the prostate but is confined to nearby tissues. This is a locally advanced stage.
- Stage 4: The cancer has progressed beyond the prostate, spreading to distant parts of the body, such as lymph nodes, bones, or vital organs.
What Are the Symptoms and Early Signs of Prostate Cancer?
Symptom severity varies based on the cancer’s location and its level of advancement. As the cancer advances to other areas of the body, the patient still may not experience symptoms.
Urinary Symptoms and Signs
- Frequent urination, especially during the night.
- Difficulty initiating or stopping urine.
- Inability to urinate.
- A weakened or interrupted urine flow.
- A feeling of incomplete emptying of the bladder.
- Terminal dribbling of the urine flow.
- Painful or burning urination.
- Blood in the urine.
- Kidney dysfunction or failure (advanced stage).
Sexual Problems
- Difficulty achieving or sustaining an erection.
- Painful ejaculation.
- Reduced ejaculation volume: Hydration, diet, ejaculation frequency, and other factors may have a more significant impact on fluid volume than prostate cancer.
- Blood in the semen.
Other Symptoms and Signs (Usually Later Stages)
- Pain or stiffness in the abdomen, lower back, spine, ribs, hips, and upper thighs.
- Swollen, weak, and/or numb lower limbs.
- Unexplained weight loss.
- Lack of appetite
- Discomfort or pain in the rectum.
- Fatigue, possibly due to anemia.
- Discomfort or pain while sitting due to prostate enlargement.
- Pain in the testicles.
What Causes Prostate Cancer?
DNA, the chemical in our cells that comprises our genes, dictates how our cells function. Certain genes play a crucial role in regulating prostate cell growth, division, DNA repair, and programmed cell death. When these genes malfunction, it can result in uncontrolled cell growth and, eventually, prostate cancer.
Inherited Gene Mutations
Inherited gene mutations found in all cells contribute to about 10 percent of prostate cancers, known as hereditary cancers. Specific genes associated with hereditary prostate cancer are:- BRCA1 and BRCA2: These genes normally assist in repairing DNA mistakes or induce cell death if repair is impossible. Their mutations are associated with an increased risk of prostate cancer.
- CHEK2, ATM, PALB2, and RAD51: These are DNA repair genes.
- DNA mismatch repair genes: These genes, including MSH2, MSH6, MLH1, and PMS2, assist in fixing DNA mistakes during cell division. Mutations can lead to Lynch syndrome, which increases the risk of prostate, colorectal, and other cancers.
- RNASEL: As a tumor suppressor gene, its normal function is to induce cell death in response to internal abnormalities. However, mutation may allow abnormal cells to survive longer, leading to an increased risk of prostate cancer.
- HOXB13: This is an essential gene for prostate gland development. Mutations in this gene have been associated with rare cases of prostate cancer at a young age in certain families.
Acquired Gene Mutations
Most gene mutations associated with prostate cancer are acquired. When prostate cells divide, errors occur during the DNA replication process, leading to defective DNA in new cells. Prostate cell growth and division speed increase the likelihood of mutations, potentially influencing prostate cancer risk. Androgens, such as testosterone, which promote prostate cell growth, might contribute to the risk, but studies have not consistently established a link between higher androgen levels and prostate cancer.Who Is at Risk of Prostate Cancer?
- Age: Prostate cancer is rare in men under age 45, constituting only 0.5 percent of all newly diagnosed cases. The prostate risk increases with age, with most cases diagnosed in men aged 50 and older. Fortunately, the cancer’s aggressiveness decreases with advancing age.
- Race: Black men in the United States have a 1.6 times higher risk of developing prostate cancer compared to white men. Caribbean men with African ancestry are more prone to developing prostate cancer than men of other races. Prostate cancer is less common in Asian American, Hispanic, and Latino men compared to non-Hispanic white men.
- Developed countries: Prostate cancer is more prevalent in developed countries, with the lowest incidence in Asian men living in Asia. However, when Asians relocate to the United States, their prostate cancer risk rises, though it remains lower than the general American male population. Prostate cancer risk is also higher among Asians residing in urban areas such as Hong Kong, Singapore, and European cities. This increase is particularly notable among sedentary men with unhealthy diets.
- Family history: A man’s risk of developing prostate cancer more than doubles if he has a father or brother with the disease. The risk is higher when a brother is affected than when a father is. The risk also significantly increases if multiple relatives, especially those diagnosed at a young age, have been affected. However, most prostate cancers still occur in men with no family history of the disease. Additionally, research indicates that having a close female relative diagnosed with breast cancer may also increase the risk of prostate cancer.
- Overweight or obesity: Studies have associated being overweight in one’s 50s and beyond with an increased risk of advanced prostate cancer. Various suggested biological mechanisms connect body fatness to cancer, including disrupted sex steroid metabolism, heightened insulin levels, and increased proinflammatory cytokines.
- Height: Taller adult height is associated with an increased risk of prostate cancer, although the specific mechanisms involved remain unidentified. Adult height may indicate factors influencing linear growth, including nutritional and genetic elements, along with cumulative exposure to hormones such as growth hormone and insulin-like growth factors (IGFs). The IGF axis is crucial in regulating cell growth and survival. One meta-analysis of over 10,000 prostate cancer cases supports a positive association between circulating IGF-I levels and prostate cancer risk. Another suggested mechanism involves taller individuals having more cells, potentially increasing the likelihood of mutations and prostate cancer development.
- Exposure to certain chemicals: According to the American Cancer Society (ACS), studies have suggested a potential association between arsenic exposure and an increased risk of prostate cancer. Additionally, evidence suggests that firefighters, due to their occupation, may be exposed to chemicals that could increase their risk of developing it. Prostate cancer is also recognized by the U.S. Department of Veterans Affairs (VA) as a disease linked to exposure to Agent Orange, a chemical employed during the Vietnam War. In addition, exposure to pesticides has been linked to an increased risk of developing prostate cancer.
- Multiple sex partners: Having multiple sexual partners throughout life or initiating sexual activity early on raises the risk of prostate cancer. However, frequent ejaculation is linked to a potential decrease in overall prostate cancer risk. Furthermore, reducing ejaculatory frequency does not increase the incidence of advanced disease.
- Sexually transmitted infections: Chlamydia, gonorrhea, and syphilis infections appear to increase the risk of prostate cancer.
- Western diet: Typically, prostate cancer is associated with the consumption of a Western diet. Such diets may include high-fat, high-calcium, and/or high-dairy diets. In a mouse model, a diet rich in lard demonstrated a notable acceleration in the progression of prostate cancer. According to the ACS, some studies indicate that men with high calcium consumption, either through foods or supplements, might face an increased risk of prostate cancer. Others propose that men with a high-fat diet, particularly rich in red meat or high-fat dairy products, may face an increased risk.
How Is Prostate Cancer Diagnosed?
- Prostate-specific antigen (PSA) test: The PSA test measures the level of PSA in the blood. The PSA is an enzyme produced by the prostate, and its elevated levels may indicate prostate cancer, although factors such as age, race, and other prostate-related conditions can also impact PSA levels. However, there is no specific threshold that can definitively determine whether a man has prostate cancer or not, and the test may yield false-positive results, suggesting cancer when it is not present, or false-negative results, indicating no cancer despite its being present. For men in their 40s, a baseline level can aid in future monitoring of any changes as long as it is correlated with the natural increase of levels with age.
- Digital rectal examination (DRE): The DRE involves a doctor inserting a lubricated, gloved finger into a man’s rectum to assess the prostate for abnormalities. However, due to insufficient evidence regarding its benefits, the U.S. Preventive Services Task Force does not recommend DRE as a screening test. Some research shows utility in situations of mildly elevated PSA levels.
Biopsy and Further Tests
In cases where PSA or DRE test results are abnormal, additional tests will be used to verify the presence of prostate cancer. A prostate biopsy is the only test that can provide a conclusive diagnosis. It involves the removal of tissue from the prostate for examination. This procedure is guided by transrectal ultrasound, utilizing a rectal probe to transmit ultrasound waves to the prostate and surrounding tissues. Typically, 12 to 14 tissue samples are taken. Since a transrectal prostate biopsy poses a risk of infection, some doctors prefer transperineal prostate biopsy, where the needle penetrates the skin of the perineum (i.e., the area between the scrotum and the anus) into the prostate instead of the rectum, thus reducing the infection risk.- Multiparametric-magnetic resonance imaging (mp-MRI): This imaging test can detect, assess, and stage prostate tumors.
- Prostate cancer gene 3 (PCA3) test: This test searches for the PCA3 gene in the urine. This gene is an extensively expressed long noncoding RNA molecule found exclusively in prostate malignancies, and larger quantities of this gene have been associated with prostate cancer.
- Prostate Health Index (PHI): This blood test calculates a score using various forms of PSA, delivering more specific results and additional information than the standard PSA test.
What Are the Complications of Prostate Cancer?
- Erectile dysfunction: Erectile dysfunction is a complication of prostate cancer and sometimes also its treatments. Over 75 percent of men may experience difficulties with erections after prostate surgery, but nerve-sparing techniques can minimize this. This condition is also common after radiation therapy and androgen deprivation therapy (ADT), with effective treatments available.
- Poor bladder control: Urinary incontinence can be caused by prostate cancer and its treatments. For instance, within one year after prostate removal, 5 percent to 10 percent of men may experience issues with urine leakage.
- Urinary urgency: Radiation therapy can lead to damage around the prostate, causing a sensation of needing to pee more frequently.
- Metastasis: Undiagnosed, untreated prostate cancer has the potential to spread to other organs, primarily through lymphatic vessels to nearby lymph nodes and eventually to bones or distant organs.
- Severe pain: Prostate cancer metastasis can result in considerable pain, particularly if cancer cells invade the bones.
- Bone fracture: In addition to bone pain, prostate cancer metastasis can also cause bone fracture.
- Spinal cord compression: This can occur due to vertebral collapse from tumor invasion into the vertebrae or tumor growth along the spinal cord. It typically occurs in the thoracic or upper lumbar spine; the main symptom is often local or nerve root pain. Compression can impair leg strength and one’s ability to walk.
- Coagulopathy and disseminated intravascular coagulation: In advanced prostatic carcinoma, patients may experience bleeding issues, ranging from manageable blood in the urine to disseminated intravascular coagulation (DIC). DIC is pronounced coagulation in vessels followed by uncontrolled bleeding.
- Anemia: Patients in advanced stages of metastatic prostate cancer frequently experience the development of anemia for unknown reasons.
- Edema: Prostate cancer can block lymphatic and venous drainage from the lower limbs and pelvis, leading to swelling in the lower extremities and genitalia.
What Are the Treatments for Prostate Cancer?
- Active surveillance is a strategy designed to prevent unnecessary treatment for non-life-threatening cancers while ensuring timely intervention for those requiring it. This approach aims to detect any signs of progression at an early stage through regular PSA tests, MRI scans, and occasional biopsies. Individuals can decide on appropriate further treatment if these assessments indicate changes or progression.
- Watchful waiting is a standard recommendation for older men when the likelihood of cancer impacting their natural lifespan is low. Additionally, watchful waiting may be advised if overall health conditions prevent the individual from undergoing any treatment.
- Surgery removes the prostate along with certain adjacent lymph nodes.
- Radiation therapy and radiopharmaceuticals: Radiation therapy uses high-energy rays to eliminate cancer cells. Radiopharmaceuticals are drugs injected into a vein containing radioactive elements that travel through the bloodstream to target cancer cells in various body parts. Once there, these radiopharmaceuticals emit radiation, effectively eliminating cancer cells in specific types of prostate cancer. Another commonly employed treatment is brachytherapy, the implantation of tiny pellets or “seeds” of radiation directly into the prostate that give off low-dose radiation within the prostate for weeks or months.
- Focal therapies are minimally invasive treatments designed to target and destroy small prostate tumors without addressing the entire prostate gland, typically applied in cases of low- or intermediate-risk prostate cancer. One focal therapy is called cryosurgery or cryotherapy, a procedure that freezes cancer cells using a metal probe inserted through a small incision between the rectum and the scrotum. High-intensity focused ultrasound (HIFU) is a heat-based form of focal therapy where ultrasound waves are directed at specific areas of the prostate with cancer using a probe inserted into the rectum.
- Hormone therapy, also known as androgen deprivation therapy (ADT), via medications or testicle removal (orchiectomy), inhibits the growth of prostate cancer, potentially slowing its progression and shrinking tumors. It is frequently combined with radiotherapy and may be prescribed post-radiotherapy to diminish the risk of cancer recurrence.
- Targeted drug therapy focuses on the specific genes, proteins, or tissue environment contributing to cancer growth and survival. Poly(ADP)-ribose polymerase (PARP) inhibitors block PARP proteins, which help repair damaged tumor cells’ DNA. The use of PARP inhibitors hinders the repair of damaged DNA in tumor cells and often causes their death. Examples of PARP inhibitors include rucaparib, olaparib, talazoparib, and niraparib plus abiraterone.
- Chemotherapy involves using drugs to eliminate cancer cells, and it may benefit men with advanced or castration-resistant prostate cancer. Treatment typically follows a specific regimen with a defined number of cycles administered over a set duration. Examples of the chemo drugs for prostate cancer are docetaxel (usually the first chemo drug given), cabazitaxel, mitoxantrone, estramustine, and carboplatin.
- Immunotherapy involves administering medications to enhance an individual’s immune system, enabling it to better identify and eliminate cancer cells. Immunotherapies may include immune checkpoint inhibitors and a cancer vaccine. These have only been shown to be effective against prostate cancer cells with specific gene mutations.
- Bone-targeted therapy may benefit men with prostate cancer that has spread to the bones, reducing the risk of skeletal-related events such as fractures and pain. Bone-targeted therapy might include corticosteroids, ablative treatments, surgery, and bisphosphonates, drugs that inhibit osteoclasts, which are bone cells that break down the hard mineral structure of bones.
How Does Mindset Affect Prostate Cancer?
- Improved emotional well-being: A positive mindset and emotional well-being may contribute to a better cancer experience for individuals dealing with prostate cancer. Through practicing stress reduction techniques and seeking emotional support, patients may be more equipped to face challenges associated with their illness.
- Treatment adherence: A positive mindset may encourage individuals to adhere to their prescribed treatment plans, as they tend to be optimistic about the effectiveness of the treatment and might experience a reduction in their fear of treatment side effects and cancer recurrence.
- Better coping: In a clinical trial involving adult cancer patients, including those with non-metastatic prostate cancer undergoing systemic treatment, participants were randomly assigned to receive the cancer mindset intervention (CMI) or treatment as usual (TAU). The CMI group, completing seven online modules over 10 weeks, showed significant improvements in adaptive mindsets about cancer and the body, leading to better overall quality of life, increased engagement in adaptive coping behaviors, and reduced distress from physical symptoms compared to the other group.
What Are the Natural Approaches for Prostate Cancer?
1. Herbal Medicines
Chinese herbal medicines are widely embraced as an alternative cancer therapy, offering benefits such as their low toxicity and ability to engage multiple pathways and targets. One review identified herbal medicine formulas, single extracts, and herbal medicine-derived compounds from several reputable online databases. These treatments demonstrated various effects on prostate cancer cells, including inducing cell death, maintenance, and cell cycle arrest, suppressing blood vessel development, proliferation, and migration, reversing drug resistance, and enhancing anti-tumor immunity.- Fuzheng Yiliu Decoction: With Astragali radix being a major ingredient, the decoction can inhibit prostate cancer cell proliferation and promote cancer cell death.
- CFF-1: This clinically utilized anti-prostate cancer herbal medicine, with Radix aconiti lateralis preparata and other herbs as its ingredients, can promote cancer cell death.
- Qianlie Xiaozheng Decoction: The decoction, containing Astragali radix, Hedyotis diffusa, and multiple other herbs, can induce cancer cell self-correction and accelerate cell death.
- Qiling Decoction: The formula, comprised of Astragali radix, Curcumae longae rhizoma, and many other herbs, can suppress prostate cancer progression and promote cancer cell death.
- Yishen Tonglong Decoction: The decoction, containing Rehmanniae radix praeparata, Astragali radix, and multiple other herbs, inhibited prostate cancer cell growth and promoted cell death in cell culture studies.
- Paridis Rhizoma: This extract can trigger prostate cancer cell death and halt the cell cycle.
- Ganoderma: This extract can inhibit the prostate cancer cells’ growth and metastatic potential, prompt cell cycle arrest, and trigger cell death.
- Trametes robiniophila: In cell culture and animal studies, it suppressed prostate cancer cell proliferation and metastasis, hindered cancer cell growth, and overcame drug resistance.
- Scutellariae barbatae herba: This extract promoted cancer cell death and halted cell cycles in a lab study.
- Curcumin: Derived from turmeric roots, curcumin inhibits the growth and spread of prostate cancer cells and induces their demise in human cell culture studies.
- Matrine: Derived from the herb Sophorae flavescentis radix, matrine and its derivatives exhibit inhibitory effects on the growth and induction of cell death in various cancer cell cultures.
- Quercetin: Quercetin, a polyphenolic flavonoid found in many Chinese herbal medicines, promotes the demise of prostate cancer cells in lab cultures and downregulates their gene expression.
- Triptolide: The active component of the herbal medicine Tripterygium wilfordii, triptolide exhibits anti-prostate cancer effects potentially linked to its modulation of the androgen receptor in lab studies.
- Astragaloside: In lab studies, astragaloside, derived from the medicinal herb Astragali radix, enhances prostate cancer cells’ susceptibility to chemotherapy drug carboplatin.
2. Diet and Nutritional Supplements
- Vitamin D: Low vitamin D blood levels are associated with an increased risk of prostate cancer development, and prostate cancer patients with vitamin D deficiencies face higher overall and cancer-specific mortality. Supplementation with vitamin D may be beneficial for such patients.
- Lycopene and vitamin E: In one mouse model, mice with prostate cancer fed lycopene and vitamin E together, each at a dose of 5 milligrams per kilogram of body weight, exhibited reduced growth of prostate tumors by 73 percent after more than 40 days. Additionally, it extended the mice’s median survival time by 40 percent.
- Cruciferous vegetables: In one prospective clinical study, men with a high intake of cruciferous vegetables had less risk of prostate cancer. Furthermore, in lab studies, the glucosinolates in cruciferous vegetables hindered growth and induced cancer cell death.
- Fish: Consuming fish may reduce prostate cancer deaths without impacting the occurrence rate. However, a high intake of dietary omega-3 fatty acids from fish oil is associated with an increased risk of prostate cancer.
- Soy: Eating more soy-based foods appears to lower the chances of getting prostate cancer, possibly because they have plant compounds called phytoestrogens that might block the 5-alpha-reductase enzyme.
3. Essential Oils
Duke University researchers found that an olfactory receptor is crucial to prostate cancer progression. This discovery suggests the potential use of essential oils, possibly via aromatherapy, to block the receptor. Certain essential oils can be developed into novel therapeutic options for treating prostate cancer, including:- Lavender: In one mouse model, lavender essential oil demonstrated efficacy in suppressing human prostate cancer growth in mice. The key contributor to this effect was linalool, and its anti-tumor impact involved inducing apoptosis and inhibiting cancer cell proliferation.
- Tree wormwood (Artemisia arborescens): In one study, researchers exposed human prostate cancer cells to two essential oils extracted from tree wormwood and discovered that the oils activated a cancer cell death process.
- Horsetail (Equisetum arvense): In a cell culture study, horsetail essential oil exhibited antioxidant activity and cytotoxicity effect on human prostate cancer cell lines, and it also increased the cell death percentage of prostate cancer cells.
4. Yoga
Incorporating stress-reducing techniques such as meditation and yoga into the care of cancer patients can support effective coping, alleviate symptoms, and improve overall health outcomes.5. Meditation
The process of diagnosing and treating prostate cancer can lead to anxiety, fear, and depression in approximately one-third of patients.6. Acupuncture
Acupuncture shows promise in alleviating cancer-related symptoms, including nausea and vomiting associated with chemotherapy, pain, and hot flashes in prostate cancer patients.How Can I Prevent Prostate Cancer?
- Eat a nutritious diet: Adopt good eating habits by incorporating fruits, vegetables, and whole grains into your diet while reducing red meats, calcium-rich foods, lipids, dairy products, and processed foods. It may be necessary to implement dietary changes many years earlier in one’s life to reduce prostate cancer risk later in life.
- Maintain a healthy weight: Since being overweight or obese increases prostate cancer risk, maintaining a healthy weight is a protective factor against the disease.
- Exercise regularly: The Health Professional’s Follow-up Study found that higher levels of exercise were linked to a substantial decrease in aggressive subtypes of prostate cancer, including advanced and fatal cases.
- Avoid promiscuity: Since men with multiple sex partners and/or certain STIs are at a higher risk of having prostate cancer, avoiding promiscuity can potentially lower the risk.
- Avoid certain chemicals: Pesticides and similar chemicals can increase the risk of prostate cancer and should be avoided.
- Consider chemoprevention: Drugs called 5-alpha-reductase inhibitors (5-ARIs), including dutasteride and finasteride, are commonly prescribed for benign prostatic hypertrophy (BPH), and they may reduce the risk of prostate cancer. According to the Prostate Cancer Prevention Trial, fewer prostate cancers were found in the group of healthy men 55 years of age and older taking finasteride compared to nonusers, with similar prostate cancer death rates. However, the group taking finasteride reported more side effects. The Reduction by Dutasteride of Prostate Cancer Events Trial (REDUCE) also investigated the potential of dutasteride in preventing prostate cancer in men aged 50 to 75. The study revealed fewer prostate cancers in the dutasteride group compared to the nonusers, with the first group reporting more side effects.
- Get PSA screenings: If discovered early, prostate cancer can be potentially cured.